Medical billing and coding is a time intensive process that requires specialized team members, representing a significant expense for medical practices. Medical billing services exist to outsource medical billing and coding so practices can focus on serving their patients instead of chasing down payments. Their expertise also helps them streamline the process with payers, reducing days in accounts receivable and boosting first pass claims rate — that all boils down to practices collecting payments sooner.
Business.com aims to help business owners make informed decisions to support and grow their companies. We research and recommend products and services suitable for various business types, investing thousands of hours each year in this process.
As a business, we need to generate revenue to sustain our content. We have financial relationships with some companies we cover, earning commissions when readers purchase from our partners or share information about their needs. These relationships do not dictate our advice and recommendations. Our editorial team independently evaluates and recommends products and services based on their research and expertise. Learn more about our process and partners here.
The Best Medical Billing Services
Your healthcare practice will benefit from a medical billing service with a first-pass acceptance rate that will get you paid sooner.

To help you find the best medical billing service for your medical practice, we conducted hundreds of hours of research and tracked the space as it has evolved over the years. We’ve chosen the following medical billing services as our best picks, each of which provides a unique value proposition to medical practices in need of revenue cycle management (RCM) support.

- Costs 4% to 8% of collections
- No long-term contracts
- 4-11-week implementation process

- Starts at $193 monthly per provider
- Medical billing software only
- 30-60-day implementation process

- Costs 3% to 7% of collections
- Three-year contract minimum
- Implementation period varies

- Costs 4% to 8% of collections
- One to two-year contract minimum
- 30-60-day implementation process

- Costs 4% to 10% of collections
- Intuitive software
- Extensive training materials
Table of Contents
At business.com, our team of technology experts has analyzed hundreds of tools and services designed to improve essential business operations, from POS systems to GPS fleet management services to remote PC access software, and we use these experiences to provide business owners with actionable guides and industry insights. Every playbook and explainer is infused with advice from real IT consultants, implementation experts, security specialists, software developers and more.
Our rigorous product review process involves in-depth industry research, vendor interviews, hands-on testing and service comparisons. Each analysis — whether for a business phone system, CRM platform, call center software or website builder — is independently verified by a business.com editor to ensure our recommendations are free of bias and errors. Learn more about our editorial process.
How We Decided
In our extensive research of medical billing services, we examined each vendor’s tools for fast, error-free revenue cycle management. We looked for providers with certified billers and coders who could sufficiently code and scrub claims, respond to payment denials...
In our extensive research of medical billing services, we examined each vendor’s tools for fast, error-free revenue cycle management. We looked for providers with certified billers and coders who could sufficiently code and scrub claims, respond to payment denials in a timely manner and coordinate with a medical practice’s in-house staff for a seamless, efficient workflow. We compared first-pass acceptance rates and medical software integrations, on top of studying monthly costs and implementation fees.
evaluated
researched
chosen
In our extensive research of medical billing services, we examined each vendor’s tools for fast, error-free revenue cycle management. We looked for providers with certified billers and coders who could sufficiently code and scrub claims, respond to payment denials in a timely manner and coordinate with a medical practice’s in-house staff for a seamless, efficient workflow. We compared first-pass acceptance rates and medical software integrations, on top of studying monthly costs and implementation fees.
evaluated
researched
chosen
Compare Our Best Picks
 | athenaCollector  | RXNT  | CareCloud  | DrChrono  | Tebra (Formerly Kareo) – MBS  | AdvancedMD – MBS  |
|---|---|---|---|---|---|---|
| Rating (Out of 10) | 8.7 | 0.0 | 8.7 | 8.6 | 8.6 | 8.5 |
| Best For | New Practices | RCM Software | Claims Scrubbing | Workflows | Tracking Claims | Ease of Use |
| Pricing | 4% to 8% of monthly collections | Starts at $193 per month, per provider (RCM software only) | 3% to 7% of monthly collections | 4% to 8% of monthly collections | 4% to 10% of monthly collections | 4% to 8% of monthly collections |
| Contract Requirement | Cancel anytime | N/A | Three-year minimum | One to two-year minimum | 60-day notice for non-renewals | One-year minimum |
| Implementation and Training | Four to 11 weeks | 30- to 60-days | Varies | 30- to 60-days | 45 days | Four to six weeks |
| Mobile App | iOS/Android | iOS/Android | iOS/Android | iOS | iOS and Android | iOS/Android |
| Review Link |
Our Reviews

- Base Price: 4% to 8% of monthly collections
- Contract Minimum: No long-term contracts. You can leave at any time.
- Implementation and Training: Implementation support and full training are included in the subscription price of the software. Expect the onboarding and implementation period to take four to 11 weeks.
We chose athenahealth as the best medical billing service for new practices because the company provides next-level consultation and coaching that can get a medical practice started on the right foot. athenahealth offers medical coding services where its HIPAA-compliant coders quickly handle burdensome coding tasks.
In addition to expert medical billers and coders, we were impressed how athenahealth provides extensive data through the athenaOne (formerly athenaNet), a database that collects information from more than 160,000 healthcare organizations that operate on athenahealth’s platform. This information can help set clear targets and key performance indicators (KPIs) for new practices to help them grow with purpose in their earliest days.

athenahealth includes a medical billing workflow dashboard that makes it easy to follow claims in real-time, even across multiple locations. (Source: athenahealth)
- athenahealth offers expert coders to support your team when managing denied claims, so you won’t have to go it alone.
- athenahealth automatically sends bills for outstanding claims and patient statements, staying on top of accounts receivable.
- athenahealth tracks data from its network of more than 160,000 healthcare providers to establish baseline metrics to help track the growth of your practice.
- athenahealth does not provide full medical billing outsourcing.
- While athenahealth’s onboarding is short, it’s fully remote.
- athenahealth’s medical software is not intuitive, and extensive training is highly recommended.
athenaCollector received a 10/10 from users who reviewed the platform on TrustRadius. Users frequently cited athenahealth’s reporting as one of the best around, and many applauded its practice management software for its front-office features. However, some users complained about the level of difficulty when creating custom reports and said the dashboard was not flexible enough.

- Base Price: Starts at $193 per month, per provider (practice management software subscription; no RCM service)
- Contract Minimum: Monthly subscription
- Implementation and Training: Implementation and training are included free with a subscription. Expect an implementation period of between 30 to 60 days.
RXNT provides exceptional medical billing software that can be used for in-house billing and coding or to run a medical billing service of your own. When testing the solution, found RXNT to be a cost-effective medical software platform that provides a viable alternative to outsourced medical billing services for practices on a budget or that prefer to keep billing operations in-house. To access RXNT’s medical billing tools, you’ll need to purchase its practice management bundle, which starts at $193 per month, per provider. However, unlike other medical billing companies we reviwed, RXNT does not offer revenue cycle management services. If you prefer to outsource your medical billing and coding, you should consider one of our other best picks.
RXNT offers user-friendly medical billing software that makes it easy to generate and track claims, adjust rejected or denied claims, review electronic remittance advice (ERAs) and more. It is suitable for a practice’s in-house medical billing and coding or managing a medical billing service’s client portfolio. Source: RXNT
| Pricing Plan | Cost | What’s Included |
|---|---|---|
| PM Bundle | $193 per month, per provider | Access to administrative software features like appointment setting, patient demographics and medical billing tools |
| Full Suite | $298 per month, per provider | Access to all the practice management features, as well as clinical tools found in RXNT’s electronic medical records software |
- RXNT offers free implementation and training, as well as weekly coaching sessions to help medical practices make the most of the platform.
- RXNT’s mobile application is supported on both iOS and Android devices.
- RXNT is competitively priced compared to other medical software platforms we’ve reviewed.
- RXNT does not offer revenue cycle management services, so you can only rely on its medical billing software to perform in-house billing and coding.
- The scalability of RXNT’s medical software is limited and may not be suitable for mid-sized and large practices or healthcare systems.
- Customer service is often hit or miss, which can be a problem when in need of a quick solution.
RXNT received an 8.0/10 from users who reviewed the platform on TrustRadius. Users liked RXNT’s medical software and data migration process. However, some users complained about slow customer service.

- Base Price: 3% to 7% monthly collections
- Contract Minimum: Three years
- Some training is included with the subscription price. The implementation period varies depending on practice size, specialty and scope of needs, but is typically 45 to 60 days.
We chose CareCloud as the best medical billing service for claims scrubbing because it relies upon a powerful billing rules engine, CollectiveIQ, that is frequently updated as payers provide new feedback about denied claims. Additionally, CareCloud provides some of the most detailed reports we found in our review, keeping its clients in the loop about health management while being MACRA compliant. CareCloud’s staff effectively works to absorb electronic remittance advice, though its first pass claims rate is among the highest we found in our review.
CareCloud also works to provide you with generative AI technology that can be used to streamline clinical, financial and operational outcomes. CareCloud’s cirrusAI offers four different solutions: cirrusAI Appeals, cirrusAI Guide, cirrusAI Chat and cirrusAI Notes. Each one assists in patient claims from the appeal reason and navigating EHR workflows to evidence-based recommendations and clinical notetaking.

CareCloud’s EMR software and practice management software seamlessly integrate, making charge entry and claim generation easy. When outsourcing your medical billing to CareCloud’s RCM service, you can track billers’ and coders’ activities directly in the practice management software. (Source: CareCloud)
CareCloud received a 9.1/10 from users who reviewed the platform on TrustRadius. Users liked CareCloud’s training support and found customer service to be prompt and helpful. However, some users complained about slow loading times and bugs that occasionally crashed the software.
- CareCloud provides practices with helpful reports on reducing claim denial and improving their cash flow.
- CareCloud does an excellent job of helping practices identify billing problems, like audit risks.
- CareCloud medical billing service is fully outsourced, from claims creation and coding to denial resolution and reporting.
- CareCloud typically requires a three-year contract minimum for most RCM clients. This is the longest minimum we encountered during our review.
- Implementation periods vary depending on the implementation tier you choose and your company size. It also requires a one-time setup fee.
- Some users have complained about slow loading times, which could be disruptive to daily operations.

- Base Price: 4% to 8% of monthly collections
- Contract Minimum: One year
- Implementation and Training: Implementation and training are included free at all subscription levels. Expect 30 to 60 days for the implementation period.
- DrChrono provides an exceptional user experience for medical practices in need of straightforward medical software tools.
- DrChrono maintains a team of medical billing and coding experts, taking the burden entirely off of medical practices.
- DrChrono’s practice management software offers full visibility into revenue cycle management services, so you can always keep tabs on your practice’s financial health.
- DrChrono had some of the longest customer support wait times we encountered in our review and often required work orders to be submitted for minor fixes.
- DrChrono’s mobile application is only supported on iOS devices.
- Medical practices with more advanced software needs may find DrChrono’s slate of features to be limited.
We chose DrChrono as the best medical billing service for workflow because its practice management software is extremely user-friendly and offers extensive RCM features. With the Apollo Plus plan, you get comprehensive coding and denial management support. Monthly reports give insight into your financial health, and denial analysis tools help you identify trends, so you can see what might be causing your claims hiccups.
For medical practices that don’t need all the bells and whistles of more cumbersome medical software, DrChrono makes things simple and efficient, regardless of which plan you choose. Drag and drop functionality for most of its tools makes the platform one of the most intuitive we encountered in our review. DrChrono also includes automated workflows for practice management functions, helping both the front office and medical billing team streamline their processes.

Posting patient payments is straightforward and intuitive with DrChrono, like most features the platform provides. Staff should require little to no training to become proficient with DrChrono thanks to its simple learning curve, meaning less disruptions and a seamless software launch. (Source: DrChrono)
DrChrono received a 9.0/10 from users who reviewed the platform on TrustRadius. The biggest standout praise from users was the platform’s ease of use and quick setup. However, others complained about lack of customization and flexibility.

- Base Price: 4% to 10% of monthly collections
- Contract Minimum: 60-day non-renewal notice
- Implementation and Training: Implementation and training are included in the subscription. Tebra offers a fast implementation period of about 45 days.
- Tebra is easy to navigate, from monitoring the company’s medical billing and coding activities to pulling up your practice’s financial data.
- Tebra offers a fast implementation process and requires no long-term contractual commitment.
- Tebra’s patient self-service tools are easy to use, provide detailed information and help drive patient satisfaction.
- Tebra’s customer service is hit or miss.
- Tebra’s system has been described as slow by some, especially when uploading documents.
- Tebra is intended for independent and new practices, and may be unsuitable for mid-sized and large practices.
We chose Tebra as the best medical billing service for tracking claims because it offers a highly navigable system for monitoring payments, from charge entry to denial management. We like how medical practices can easily keep tabs on everything when outsourcing their medical billing to Tebra, an important aspect of quality assurance when it comes to a medical practice’s financial well-being.
We also were impressed with Tebra’s real-time reports, which are updated 24/7 and provide an instant window of visibility into all your practice’s fiscal data. Although Tebra doesn’t provide its own revenue cycle management (RCM) services directly, its features have been shown to improve revenue management by almost 10 percent for its clients.

Tebra’s medical billing tools include a patient self-pay option which can help you collect outstanding co-payments with ease. Patients receive a receipt that includes a breakdown of services, so they can always understand what they were charged for and why. (Source: Tebra)
Tebra received a 6.9/10 from users who reviewed the platform on TrustRadius. Tebra users cited the medical software’s ease of use as a major selling point. Others complained about disruptive bugs and crashes, however.

- Base Price: 4% to 8% of monthly collections
- Contract Minimum: One year
- Implementation and Training: Implementation and guided training are included. Free two-day on-site implementation is available for practices with more than $200,000 in monthly collections.
AdvancedMD is our choice for the best medical billing service for ease of use because its practice management software combines a powerful slate of features with superb usability. We were impressed with how easily medical practices can track the activity of AdvancedMD’s billing with customizable and scalable software that can meet the needs of any growing healthcare organization. We also liked that the company provides custom bundles tailored to practices’ unique needs, with discounts of up to 40 percent, making it cost-effective and worthwhile to devise your own plan.

AdvancedMD excels at displaying important information at a glance, especially on its flexible, customizable dashboards. The example above shows a dashboard that’s been configured to display financial data and important medical billing and coding news. Source: AdvancedMD
AdvancedMD received a 9.7 out of 10 from users who reviewed the platform on TrustRadius. Users most often liked AdvancedMD’s thorough implementation and wide range of features. However, some complained about lackluster customer support.
- AdvancedMD maintains a robust code library that’s up to date with the latest medical coding standards.
- AdvancedMD offers built-in connections with major clearinghouses to further streamline the billing process.
- AdvancedMD’s medical software offers extensive features and is highly scalable for growing medical practices.
- AdvancedMD may not be suitable for behavioral health specialties.
- AdvancedMD is one of the more expensive platforms we reviewed.
- AdvancedMD’s implementation period was among the longest we encountered in our review of medical billing services.
What is Medical Billing?
Medical billing is the process by which claims are generated, coded and submitted to payers like insurance companies. Medical billers then monitor these claims and handle rejections, denials and adjustments. Medical billing also involves the creation of patient statements for collecting any out of pocket expenses a patient may owe.
Unlike many other businesses, medical practices don’t get paid at the time services are rendered. Instead, they need to work with insurance companies to collect payments. This can take 30 days or more depending on the efficiency of the billing department and how quickly payers react to claims. A sluggish medical billing department can lead to significant problems for a medical practice’s cash flow.
How Does the Medical Billing Process Work?

The medical billing process begins before the encounter, when front office staff captures patient details and verifies their insurance. During the encounter, providers complete a patient’s chart, which includes services rendered during the visit. Then, medical coders and billers take over, creating claims and submitting them to payers. They will follow up on any denied or rejected claims, as well as handle patient billing for out-of-pocket expenses and copayments.
Here’s a general overview of the typical medical billing process from start to finish.
- Patient registration: Collect patient information and insurance details
- Insurance verification: Check coverage and eligibility
- Service documentation: Record medical services provided
- Charge entry: Convert services into billable codes (CPT, ICD-11)
- Claim generation: Create and submit claims to insurance companies
- Payment posting: Record payments received from insurers and patients
- Follow-up: Address denied or partially paid claims
- Patient billing: Bill patients for remaining balances after insurance
- Reporting: Analyze financial performance and identify areas for improvement
What Are the Benefits of Using Medical Billing Software?
When you choose the right medical billing service, you’ll notice a range of benefits almost immediately. These include faster payments, improved organization and reduced errors.
- Streamlined back-office processes: Outsourcing to a medical billing service reduces the staff and resources your practice must expend on back-office processes like billing and coding. Because these services minimize the administrative burden on your staff, they have been known to reduce burnout in the healthcare field.
- Payment tied to success: A medical billing service’s payment is connected to the success of your practice, since it generally costs a percentage of your monthly collections to outsource to an RCM service. The more money a medical billing service successfully collects on behalf of your practice, the more it gets paid, so it is invested in helping you succeed.
- Faster reimbursements: Medical billing services are experts in coding and billing, so they can typically navigate the process much more easily than a single practice can. This is especially true if the RCM service has an existing relationship with clearinghouses and payers. This means less waiting around for payment on the services you’ve already rendered.
- Lower denial and rejection rates: With its knowledge of payers’ expectations and advanced claim-scrubbing software, a good medical billing service should immediately reduce the rate of your claims’ denial or rejection by payers. Look for a first-pass claims rate above 95% to be sure you’re partnering with an effective RCM service.
- Patient statements and follow-up: Medical billing services don’t just deal with insurance companies; they also manage your patients’ statements. Whenever a patient owes money out of pocket and hasn’t paid in your office, your medical billing service will send them a statement explaining their bill. If the bill goes unpaid, the billing service will follow up with the patient. In extreme cases, a medical billing service may even refer unpaid accounts to a collections agency.
- Detailed financial reporting: Many medical billing services capture all the data related to your claims and couch it in easy-to-filter reports. The level of reporting and the usefulness of the visualizations vary by company, but this full accounting of your practice’s finances can be extremely helpful.
- HIPAA compliance: By law, medical billing services must comply with HIPAA security and privacy laws. When you partner with a top medical billing service, you can rest easy knowing sensitive patient and financial data is secure.
How Much Will Medical Billing Services Cost?
Pricing models are primarily the same from company to company in the medical billing industry. Most companies in our review charge a percentage of your net monthly collections, meaning the more revenue they generate for you, the more they get paid. Those percentages typically fall between 3% and 9%, although there are outliers on both ends.
Some companies charge additional fees, such as setup, implementation or clearinghouse fees. These fees can vary greatly by company, so it’s important to ask sales representatives about their companies’ policies.
Occasionally, medical billing services will institute a monthly minimum in case the practice’s revenue for the month isn’t high enough to be profitable for the billing company. Other services charge a monthly per-provider base price, taking a small percentage of collections on top of that, but this model is rare.
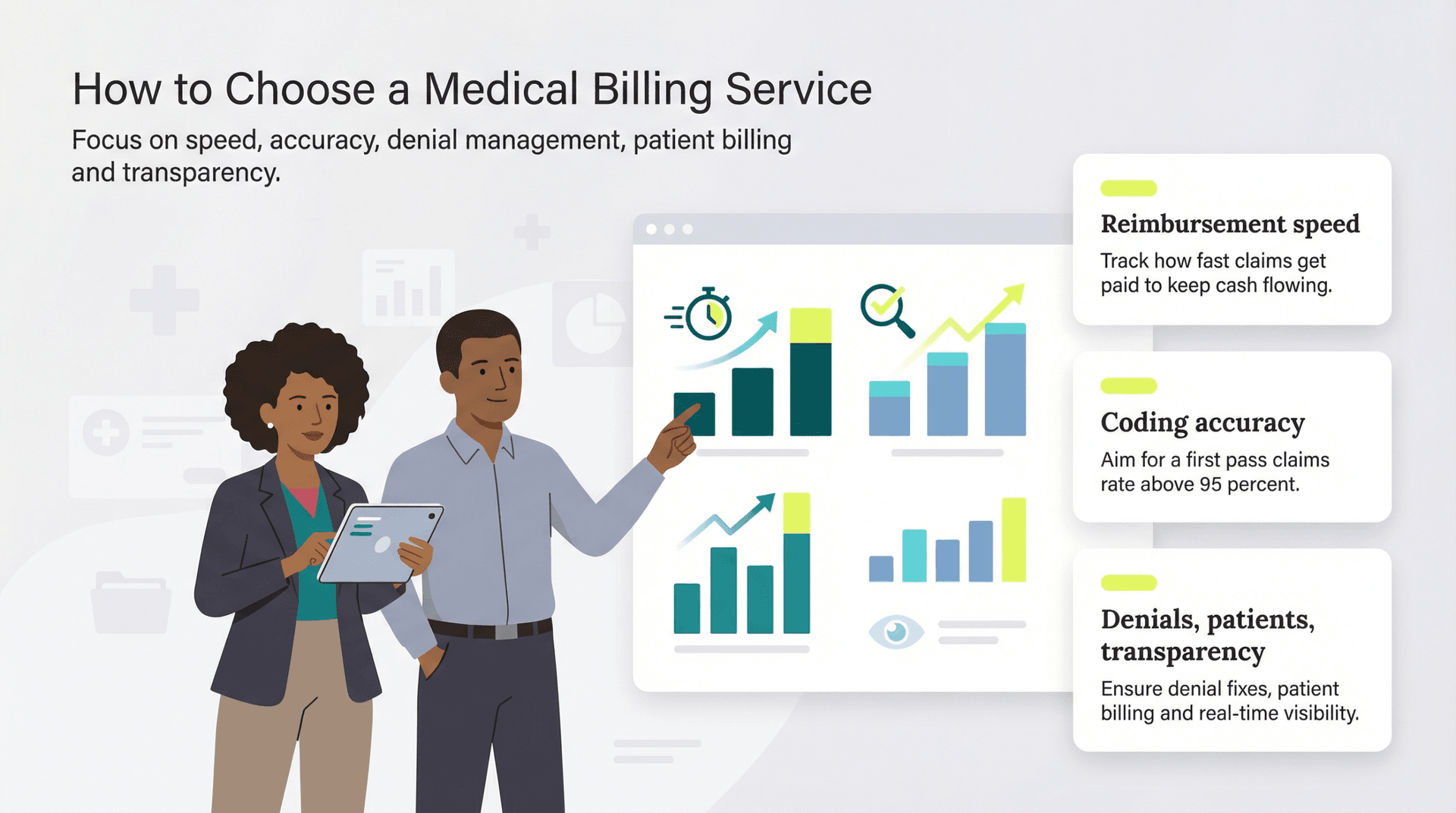
How to Choose a Medical Billing Service
Choosing the right billing service means interrogating every aspect of their process before signing a contract. A medical billing service will be handling your money and highly sensitive patient data, so you should have the utmost trust and confidence in a service before you hire them.
“From my experience and understanding, the must-have features are robust claims processing, coding accuracy, and compliance with regulations like HIPAA,” said John Russo, vice president of Healthcare Solutions at OSP. “Effective denial management and patient-friendly billing systems are essential to ensure financial stability and improve patient satisfaction.”
Consider average reimbursement time
When choosing a medical billing service, compare them to your existing billing department with specific metrics like reimbursement time. The sooner you get paid, the stronger your cash flow, which is a major factor in a small business’s survival. A medical billing service should significantly improve upon your current average reimbursement time.
“I worked on a project where we streamlined the submission of insurance claims, significantly reducing the time it took for reimbursements to come through,” Russo said.
Consider coding accuracy and first pass claims rate
Medical coding is critically important when it comes to getting claims paid quickly and on the first pass. Scrutinize a medical biller’s track record when it comes to medical coding and first pass claims rate before hiring them. If their medical coding is up to par, their first pass acceptance rate should exceed the industry standard 95 percent.
“Another essential function is coding accuracy. Proper coding ensures correct billing services,” Russo said. “In one of my recent projects, we implemented a system that automatically checked for coding errors, which cut down on claim denials by 25 percent.”
Review denial management processes
The ability to revise claims and turn denials into collections is the hallmark of an effective billing department. To be able to do so quickly and efficiently is even more important. Review a service’s denial management process to determine how quickly you can expect them to fix errors and get claims paid.
“Denial management is also crucial. Handling rejected claims efficiently can save much revenue,” Russo said. “In a recent project, we created a module that flagged and provided detailed reasons for denied claims, making it easier to address issues quickly.”
Don’t forget about patient billing
It can be easy to focus on dealing with the payers and asking billing services how they’ll manage following up on denied claims, but patient billing is just as important. Collecting copayments at the point of care is a big part of it, but oftentimes you’ll need to send patient statements for out-of-pocket expenses after the fact. Patients may sometimes be slow to pay when receiving a statement well after their appointment, so a robust and prompt patient billing process is critical.
“Patient billing and collections are equally important. Clear, accurate bills and efficient follow-up on unpaid bills help maintain a healthy revenue cycle,” Russo said. “I’ve seen firsthand how a patient-friendly billing system can improve collections and patient satisfaction.”
Consider transparency in medical billing software
When you outsource your billing to a RCM service, you should still be able to monitor everything the team is doing in real-time. Before signing a contract, be sure you can see what coders and billers are doing on your behalf in your practice management software. You may have to switch to a new platform for certain medical billing services, as well, but others could integrate with your existing medical software suite.
What Are Some Services a Medical Biller Provides?
Medical billing services allow practices to outsource their medical coding and billing processes. Also known as revenue cycle management (RCM) services, medical billing companies remove the burden of coding claims, submitting them to payers, following up on unpaid claims and managing denied claims.
Outsourcing your RCM puts a dedicated team in charge of generating your claims, scrubbing them for errors and chasing denials or underpayments, which reduces or eliminates the workload associated with in-house billing. Best of all, most services operate directly within your clinic’s existing practice management software, allowing your staff to monitor the progress of your submitted claims.
While medical billing services offer significant benefits, it’s important to choose the right one for your practice. The wrong partner could tie up your practice’s money and possibly allow patients’ payments to fall through the cracks. To ensure smooth cash flow, medical billing departments need to capture charges and create claims for them quickly, properly code those claims, and submit them through the right channels to the proper payers. Even as new charges come in, the billers must keep tabs on previously submitted claims in case they are rejected or denied by payers. If they are, the billers must revise and resubmit those claims – without falling behind on the new claims. Medical billers are also responsible for sending statements to patients for copayments or out-of-pocket expenses and following up on unpaid patient accounts.
The challenges of medical RCM require billing departments to be nimble and adaptable. They must stay abreast of updates, such as changing regulations and shifts in payers’ policies. No matter which way you slice it, in-house medical billing demands a lot of time, energy and money. That’s why many medical practices outsource the process to third-party medical billing companies, sometimes called RCM services.
What Are Some Alternative Medical Billing Services?
Not convinced that one of our best picks is the right medical billing service for you? Check out these alternative options that are worth considering if you’re looking to outsource your revenue cycle management to a reliable partner.
ChartLogic
ChartLogic is a medical billing service dedicated to making the onboarding and training process as simple as possible. The entire onboarding process takes no longer than six weeks and is meticulously customized for your practice. Training is quick and straightforward, and the interface is user-friendly. Users can start using the software right away. Support staff is available for ongoing support and challenges. ChartLogic is perfect for the tech-panicky individual. ChartLogic has all the EHR tools necessary to make your practice, including your billing, run as smoothly and efficiently as possible. Office managers use its practice management tools to handle appointment scheduling, reporting and claims, while billing specialists use its functions to determine eligibility and manage collections.
CureMD
CureMD offers one of the most intuitive, flexible dashboards for setting and tracking your practice’s key performance indicators (KPIs). Regardless of your practice’s specialty or size, you can adjust its KPIs and targets, and then track their progress as CureMD performs charge entry, coding, claim submission and denial management. CureMD is a low-cost medical billing service starting at a price of 4% of your monthly collections, which is more cost-effective than many of the medical billing services we reviewed, whose rates can range from 5% to 10% of monthly collections. CureMD also supports more than 30 specialties, making it a good fit for a wide range of medical practices. Certain specialties have unique needs, such as specific ICD-10 codes or payer rules.
MedicsPremier
MedicsPremier, a software platform and medical billing service from the Advanced Data Systems Corporation (ADSC), is an effective choice for growing practices looking for a competitively priced solution. For one thing, MedicsPremier begins your service with a test run on 50 to 100 patients, ensuring all vital elements of your billing operations (such as insurance eligibility verification and patient statements) are running smoothly. This is key for scaling operations, helping you guarantee your systems won’t break when your claims volume increases. MedicsPremier’s pricing is on par with other billing services we reviewed. Ranging from 3% to 6% of your monthly collections, based on the specialty and claims volume of your practice, MedicsPremier beats the industry-standard pricing we discovered in our research.
Methodology
To determine the best medical billing service on the market, our team of billing experts evaluated an initial list of 15 service providers. Our experts and analysts studied each provider’s plans and services to evaluate their medical billing operations on more than 20 factors. After this initial round of research, we narrowed down our list of candidates and identified the services we wanted to review even more closely.
After whittling our list down to 11, we scheduled Q&A sessions with medical billing service specialists so we could get a better sense of how each company operated. After analyzing each against the criteria below, our expert reviewers ultimately chose six medical billing services as our top recommendations.
These factors were broken down into categories and were weighted differently in our overall conclusion. The weights were determined based on how much business owners prioritize these criteria when shopping for business software and services and making purchasing decisions.
- Pricing (30%): Our experts and analysts compared and contrasted each vendor’s plans, judging which packages offered the best bang for your buck. We took into account monthly subscription costs, contract requirements and additional fees.
- Features (25%): We looked for standard medical service functions like coding and charge entry, claims scrubbing, clearinghouse integrations and rejection and denial management. We also considered the medical billing software each provider worked within, and looked for services that offer flexibility to use the platforms you prefer.
- Ease of Use (20%): We tested the medical software that each medical billing service works within to determine how easy it was to use. This included navigation of the interface, use of key features and accessibility of key reporting metrics.
- Implementation and Training (15%): We considered the level of implementation and training support available, especially if a medical billing service requires practices to switch its medical software. Data migrations and set up of these systems can be complex and time consuming, so we prioritized medical billing services that would also help implement software and train staff on how to use it.
- Customer Service (10%): We evaluated the range of customer service options, including whether phone assistance was provided with all package tiers. We placed extra emphasis on medical billing services that provide a dedicated account manager as a point of contact.
Based on these criteria, we not only determined which medical billing services our readers could trust but also the ways in which each solution could best serve different business needs. Some platforms were better at certain tasks than others or more suited to a particular type of company. These takeaways informed the “Best for” use cases you see on this page.
To learn more about our methodology, see our full editorial process.
FAQs
Yes, you can outsource medical billing to a third-party service, sometimes called a revenue cycle management (RCM) company. If your billing team is overwhelmed or underperforming, outsourcing to an RCM service could be a way to get claims paid more quickly and reduce your rate of denials and rejections.
For patients whose payer is Medicare or Medicaid, the 72-hour rule governs the period before hospital admissions. Any outpatient diagnostic or other medical services that occur within 72 hours prior to hospital admission must be billed alongside hospital costs. Any RCM companies you hire for your practice should be familiar with this rule.
Yes, there is free medical billing software out there. However, we recommend paying for one of the best medical software platforms to ensure patient and financial data remains secure. Free solutions are unlikely to have the same level of security or customer support as a paid platform, making them well worth the investment. Data breaches or system crashes could end up costing much more than the subscription price of reliable software in the long run.
What to Expect in 2026

Through 2032, the medical billing outsourcing market is projected to expand at a compound annual growth rate of 12.3 percent, according to Data Bridge Market Research. This growth indicates an increasing trend among solo practitioners and small practices to outsource billing operations as a strategy to reduce overhead and eliminate labor-intensive, in-house processes. Industry projections suggest the medical billing service sector could reach a market value of $40.1 billion by 2032. In 2026, we expect this outsourcing trend to accelerate.
In 2025, artificial intelligence made significant strides in medical billing. Companies like Outbound AI introduced generative AI technology to reduce administrative burdens on billing staff. Through AI-powered tools including ChatGPT, staff can now more efficiently manage denials, process EOBs and verify eligibility and benefits.
Security remains paramount following several high-profile breaches. The October 2023 Arietis Health breach exposed patient data including medical information and Social Security numbers on the dark web. The February 2024 ransomware attack on Change Healthcare, a UnitedHealth Group unit, further emphasized cybersecurity’s critical importance. In 2026, expect medical billing services to significantly strengthen their digital security measures while encouraging practices to do the same.
Medical billing quality standards are increasingly scrutinized. A December 2023 study revealed that 62 percent of U.S. hospitals failed to meet at least one of three essential billing standards: timely itemized statements, appropriate legal action timing on unpaid bills and patient access to qualified billing representatives. Medical billing services are prioritizing these measures for both hospitals and smaller health systems throughout 2026.
Transparency in medical billing continues to gain momentum through both consumer advocacy and legislative action. In Texas, recent legislation mandates that hospitals provide clear, itemized invoices before sending patients to collections. Colorado’s Division of Insurance is investigating billing errors potentially affecting thousands of patients. Minnesota’s Attorney General conducted public listening sessions in 2024 as part of investigations into major health systems’ billing practices. These developments signal that transparent, patient-friendly billing will remain essential in 2026.
Medicare coverage continues expanding, requiring billing services to adapt. The Centers for Medicare and Medicaid Services (CMS) broadened Medicare dental coverage, which now covers dental services essential to patient treatment and disease outcomes. This includes coverage for treatments eliminating infections before organ transplants and certain cardiac procedures. Billing services must continuously adapt to these coverage shifts to remain effective in 2026.
